Your go-to destination to discover practical strategies. No matter where you are in your professional journey, you'll find something valuable here.
360 Neuro Health Blog
More on the vestibular ocular reflex (VOR)
The vestibular ocular reflex (VOR) acts to maintain stable vision during head motion. This is successfully accomplished through precise compensatory eye movement to head movement along three axes via neural pathways more commonly known as the angular and translational VOR. The angular VOR (a-VOR) is mediated by the semicircular canals (SCCs) and is the primary neural pathway responsible for gaze stabilization. The linear VOR, on the other hand, is mediated by the otolith organs and compensates for translation (t-VOR). The t-VOR is most important when the head is moving at relatively high frequencies while we are viewing near targets. For now, we will limit our discussion to the a-VOR.
To better understand the VOR function, we will briefly review the role of the extraocular muscles. There are six extraocular muscles that contribute to eye movements, which reside in planes that are approximately parallel to the plane of their respective SCCs. The SCCs are responsible for facilitating muscles on the same side and inhibiting muscles on the opposite side to mediate the a-VOR. These compensatory eye movements stabilize images on the fovea and allow for clear vision during head movements, which is known as gaze stabilization. The difference between the eye and corresponding head movement is the VOR gain. Ideally, the gain of the VOR is 1.0, meaning there is a compensatory eye velocity equal to the head velocity and in the opposite direction. For example, if the head turns 30°/sec to the right, then the eyes turn 30°/sec to the left to maintain stability of the image on the fovea.
Dysfunction in the VOR affects the gain, resulting in a decline of dynamic visual acuity with brief rapid head movements, quick turns, and even in driving1. A VOR impairment may cause symptoms of dizziness, unsteadiness, and nausea. In more severe VOR dysfunction, the individual may experience oscillopsia — the sensation that objects are jumping or moving during head movements. The VOR remains sensitive and vulnerable to any type of peripheral or central vestibular disorder. VOR dysfunction can also occur with migraines, anxiety, and mood disorders.
Clinical VOR Tests
The following describes the 3 most common quick bedside clinical tests for the a-VOR.
Head Thrust
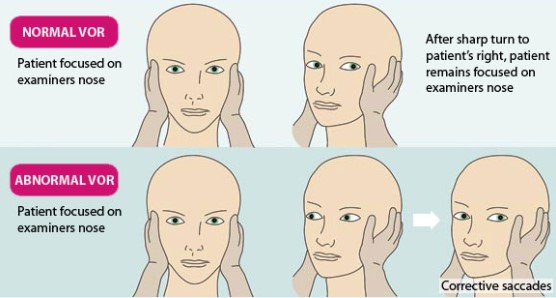
The head thrust test is a single, rapid head turn based on the oculocephalic reflex, or “Doll’s Eye” reflex, which is performed as a standard for individuals who are in a coma or unresponsive. The head of the patient is rapidly turned in the horizontal plane to one side (∼30°), while the clinician observes for compensatory conjugate eye movements in the opposite direction. Halmagyi and Curthoys originally expanded the clinical application of this test to conscious patients with unilateral vestibular loss2. The test is considered positive (abnormal) if the examiner observes a corrective eye movement, or saccades, back to the target (typically the examiner’s nose) from the rapid head movement and is shown in Figure 1 below. Although the head thrust test may provoke symptoms (e.g., dizziness) in individuals with vestibular dysfunction, corrective saccades due to retinal slippage are rarely observed in the clinical setting unless the injury involved significant unilateral vestibular dysfunction or if the patient is being evaluated in the acute stages of vertigo.
Head Shake
The head shake test is used to identify the possibility of asymmetrical vestibular input due to peripheral or central pathology. The examiner passively performs head oscillations, or the subject does so actively. Head oscillations should occur with head flexion of ∼20° to align the horizontal canals parallel to the ground and cover a 60° arc (30° side to side) at 2 Hz (2 cycles/s) for 20 repetitions. The higher velocity of the head movement exceeds pursuit system, which can only maintain gaze stabilization up to 1 Hz. Normally, no nystagmus is expected. Some individuals with peripheral or central vestibular dysfunction show a transient nystagmus (∼30 seconds) with the fast phase toward the unaffected ear after the head movement is stopped4. A slower nystagmus that switches directions may follow. This test has improved sensitivity with Frenzel goggles or infrared video goggles, but it has low sensitivity overall as a screening tool for vestibular dysfunction, especially without the use of goggles to suppress fixation5.
Dynamic Visual Acuity
The DVA test was originally discussed in 1984 for assessing vestibular loss and has since become a standard clinical test for vestibular therapists6. The test is performed in the sitting position, and the individual wears corrective lenses as needed. The individual reads the lowest line on a visual acuity chart (eg, Snellen chart), recording the smallest line read with less than three errors (eg, 20/20). The examiner flexes the patient’s head by 20º and continues to hold the patient’s head with both hands and rotates it back and forth in the horizontal plane in a 40°–60° arc (20°–30° side to side to side) at ∼2 Hz (exceeding compensation by the pursuit system), all while the patient reads the visual acuity chart while the head is moving.
Of note to the reader is that authors frequently reference hertz when describing the methodology in assessing the VOR, especially with the DVA test. Yet, the VOR doesn’t operate based on the frequency of head movement. It works based on the velocity of the head movement.
Kamran Barin, PhD, provides the following example: “If your head is moving about +10 degrees, your head velocity right at the point where it’s passing the center is about one hundred twenty-five degrees per second. If your excursion or amplitude is + 20 degrees, your head velocities are now around two hundred fifty-one degrees per second7.”
Dr. Barin further notes the problem in this scenario is the risk of error when we’re trying to translate velocities into frequencies because we can get a large difference in values of degrees per second based on small differences in head amplitude. It is important for the examiner to know the individual’s visual acuity will be affected by the amplitude of the head movement must be considered when performing the DVA and when prescribing VOR exercises for the patient.
Most clinicians will utilize a metronome to time the head movements. If the examiner is following the guidelines of +20 degrees, the metronome would be set to 120 bpm and the patient would complete a full cycle to each beat or set the metronome to 240 bpm if asking the subject to change head direction to each beat. In the video below, Dr. Barin further discusses DVA testing:
Dr. Kamran Barin serves as one of our Certificate of Competency in Vestibular Rehabilitation (CCVR) Course faculty members. Dr. Barin is Assistant Professor Emeritus at the Department of Otolaryngology Head and Neck Surgery and Department of Speech and Hearing Sciences at The Ohio State University. He established and served as the director of the Balance Disorders Clinic at The Ohio State University Medical Center for over 25 years until his retirement in June 2011.
Because of Dr. Barin’s research and consulting in the development of vHIT and Bertec Vision Advantage (BVA), we are constantly picking his brain about the research regarding VOR assessment and rehabilitation. As we mentioned to him on several occasions, one of the most common questions (or perhaps discrepancies) we encounter is: what is the proper technique and/or best method for performing the dynamic visual acuity test?
Sensitivity and specificity of the DVA test varies greatly, as a result of varied methodology, such as passive (examiner moves head) versus active (subject moves head) oscillations, frequency of head movements, amplitude (size) of head movement, and whether the patient is trying to read when going towards the affected side versus unaffected side. Additionally, it is recommended to perform DVA testing with the head tilted 20° into flexion to isolate the horizontal canal yet vision can be obscured for those wearing corrective glasses, plus the overall range of visual acuity diminishes in upward gaze. A normal result is more than a one-line change in younger individuals or more than two lines in older individuals8-9.
The examiner should also ask about a provocation of symptoms, which is considered abnormal if persistent beyond a few seconds from stopping the test. As noted in Dr. Barin’s interview and as shown in several studies, computerized VOR testing provides more objective and reliable information regarding VOR gain as well as information on phase (timing) and symmetry. More sophisticated VOR testing is typically conducted in specialized dizziness and balance centers. Rotary chair testing assesses VOR function at slower speeds, which are less correlated with dynamic activities performed in daily living (e.g., walking, turning, etc.) and especially those demands associated with sports-related activities. High-velocity head rotation testing can better assess higher demands of VOR function. These head rotation systems have more recently incorporated the use of infrared video goggles or an inertial measurement unit (IMU) head sensor versus the use of electrodes. Some systems (such as the computerized head thrust test) can measure smaller corrective saccades (covert saccades) while others can identify at what velocity the VOR becomes inefficient, which indicate vestibular disruption.
Advanced VOR testing holds the potential to identify subtle dysfunction in the vestibular system, especially if the individual reports vestibular symptoms but traditional vestibular diagnostics (rotary chair or caloric testing) is normal. More reliable and objective VOR testing helps identify impairments that are not otherwise observable in the clinical exam and aids in developing the most appropriate treatment plan. The potential to rehabilitate the VOR to decrease, if not alleviate, vestibular-related symptoms is high yet is context-specific. Treatment plans that focus on discrete, measured impairments are more efficient and more likely to produce optimal results. Objective data to guide the patient’s care plan can also be used to monitor progress, customize treatment, document effectiveness, and add to patient motivation. Outcome studies have established that a customized approach results in better outcomes than general approaches.
REFERENCES:
- (MacDougall and Moore, 2005)
- Halmagyi GM, Curthoys IS. A clinical sign of canal paresis. Arch Neurol. 1988;45:737–739.
- BMJ Best Practice. A delicate balance: managing vertigo in general practice. BMJ; 2012. Available from: https://bpac.org.nz/BPJ/2012/September/vertigo.asp (Accessed October, 2019).
- Hain TC, Fetter M, Zee DS. Head-shaking nystagmus in patients with unilateral peripheral vestibular lesions. Am J Otolaryngol. 1987;8:36–47.
- Jacobson GP, Newman CW, Safadi I. Sensitivity and specificity of the head-shaking test for detecting vestibular system abnormalities. Ann Otol Rhinol Laryngol. 1990;9:263–271.
- Longridge NS and Mallinson AL. The dynamic illegible E-test. A technique for assessing the vestibular-ocular reflex. Acta Otolaryngol. 1987;103:(3–4):273–279.
- Barin K. interview
- Dannenbaum et al. Optimal parameters for the clinical test of dynamic visual acuity in subjects with unilateral vestibular hypofunction. Otol Neurotol. 2009;30:368.
- Dannenbaum et al. Optimal parameters for the clinical test of dynamic visual acuity in patients with a unilateral vestibular deficit. J Otolaryngol. 2005;34;13.